Often dubbed the “feel-good” neurotransmitter, serotonin is recognized primarily for its role in regulating mood, anxiety and emotional well-being. However, its influence extends far beyond the confines of mental health; this important chemical messenger significantly impacts cardiovascular health as well. Here, we will explore the intricate relationship between serotonin deficiency and cardiovascular health, including the link between low serotonin and heart disease.
Understanding Serotonin: A Multifaceted Neurotransmitter
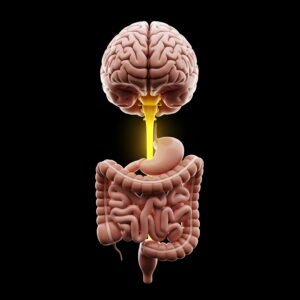 Serotonin, chemically known as 5-hydroxytryptamine (5-HT), is a neurotransmitter that plays a vital role in a wide range of physiological processes. While a small portion of serotonin is found in the brain, approximately 90% resides in the gastrointestinal (GI) tract, where it regulates bowel movements and overall digestive function.
Serotonin, chemically known as 5-hydroxytryptamine (5-HT), is a neurotransmitter that plays a vital role in a wide range of physiological processes. While a small portion of serotonin is found in the brain, approximately 90% resides in the gastrointestinal (GI) tract, where it regulates bowel movements and overall digestive function.
Beyond its well-known role in mood regulation, serotonin influences several other bodily functions, such as sleep, appetite and cognition. It serves as a precursor to melatonin, the hormone responsible for regulating sleep, and helps control food intake while influencing feelings of satiety. Additionally, serotonin affects learning and memory. Given its extensive role in the body, serotonin deficiency can lead to various issues that impact both physical and mental health.
The Link Between Serotonin and Cardiovascular Disease
As previously discussed, serotonin is a versatile neurotransmitter that affects more than just mood and digestion. While serotonin is best known for its role in regulating emotions and gut function, studies show it also plays an important part in heart health. Serotonin influences various aspects of the cardiovascular system, including blood vessel function, heart rate and blood pressure regulation. Below are detailed just some of the ways in which serotonin impacts heart health.
Vascular Function and Regulation
Serotonin plays a major role in controlling the function of vascular smooth muscle cells, which affects how blood vessels constrict and relax. This process, known as vasoconstriction and vasodilation, is essential for maintaining healthy blood pressure. When serotonin levels are balanced, blood vessels function properly, allowing adequate blood flow and oxygen delivery to various tissues in the body. However, if serotonin levels drop, this balance can be thrown off. A serotonin deficiency can lead to increased blood pressure because the vessels may have trouble relaxing, resulting in a condition known as hypertension. Over time, hypertension can heighten the risk of serious heart-related problems, such as heart attacks and strokes.
Low serotonin levels can also lead to problems with the endothelium, which is the thin layer of cells that lines blood vessels. When the endothelium doesn’t function properly, it can pave the way for atherosclerosis, a condition where arteries harden and narrow. This hardening restricts blood flow, making it harder for the heart to deliver blood to the rest of the body.
Serotonin and Inflammation
Chronic inflammation is a known contributor to heart disease, and recent research suggests that serotonin plays a key role in managing the body’s inflammatory response. When serotonin levels are low, inflammation in the body may increase, leading to higher production of cytokines; signaling molecules that can trigger further inflammation. Elevated cytokine levels can damage the endothelium, the layer of cells lining blood vessels, which compromises their function. This damage paves the way for atherosclerosis, a condition where fatty deposits build up in arteries, narrowing them and restricting blood flow.
Additionally, ongoing inflammation can create a cycle that further raises cardiovascular risks. Persistent inflammation may lead to increased oxidative stress, which harms cells and tissues throughout the cardiovascular system. Not only does this oxidative damage speed up the progression of atherosclerosis but it can also lead to the formation of blood clots, increasing the risk of heart attacks or strokes.
Understanding how serotonin deficiency relates to inflammation and heart health could open up new treatments aimed at lowering the risk of heart disease. By improving serotonin levels and managing inflammation, we may discover effective strategies to reduce the negative effects of chronic cardiovascular problems.
Heart Rate and Arrhythmias
Serotonin plays a key role in regulating heart rate through its actions on the autonomic nervous system, which controls involuntary bodily functions like heart rhythm. Serotonin influences both branches of this system—the sympathetic and parasympathetic nervous systems—helping the heart respond to various physiological conditions. When serotonin levels are balanced, it helps maintain a stable heart rate. However, when serotonin levels drop, the risk of developing arrhythmias—irregular heartbeats—increases.
 Arrhythmias can vary in severity, from mild cases that go unnoticed to serious situations that can affect how well the heart pumps blood. People with arrhythmias may feel symptoms like palpitations, dizziness or fainting, especially during exercise. This is especially concerning for those with existing heart conditions, as arrhythmias can worsen these issues and lead to serious complications like heart failure or stroke.
Arrhythmias can vary in severity, from mild cases that go unnoticed to serious situations that can affect how well the heart pumps blood. People with arrhythmias may feel symptoms like palpitations, dizziness or fainting, especially during exercise. This is especially concerning for those with existing heart conditions, as arrhythmias can worsen these issues and lead to serious complications like heart failure or stroke.
Research indicates that the interplay between serotonin levels and heart rhythm is nuanced. Low serotonin may not only disrupt normal heart rhythms, but it can also change how electrical signals travel through heart tissues, further increasing the risk of arrhythmias. Additionally, low serotonin can increase anxiety and stress, which can also negatively impact heart health. Given these critical roles, keeping serotonin levels in check could be vital in managing heart rate and reducing the risk of arrhythmias, ultimately improving heart health.
The Psychological Connection
Serotonin deficiency is most famously linked to mood disorders, particularly depression and anxiety, which significantly impact cardiovascular health in several ways. Individuals suffering from depression often engage in unhealthy behaviors, such as poor diet, lack of exercise and smoking, all of which can adversely affect heart health. These behaviors may stem from the low motivation and energy levels characteristic of mood disorders, ultimately increasing the risk of cardiovascular disease. Additionally, chronic stress associated with these mood disorders can lead to elevated levels of cortisol and other stress hormones. Prolonged exposure to these hormones can exacerbate hypertension, increase heart rate and elevate the overall risk of cardiovascular issues. Understanding these interconnected factors is essential for developing comprehensive treatment strategies that address both psychological well-being and cardiovascular health.
Clinical Implications and Strategies
Understanding the connection between serotonin levels, mood disorders and cardiovascular health is essential for effective clinical practice. Healthcare providers should consider evaluating serotonin levels, particularly in patients presenting with both cardiovascular symptoms and mood disturbances. Pharmacological interventions, such as serotonin reuptake inhibitors (SSRIs), may offer both mood support and cardiovascular benefits. Additionally, lifestyle modifications—like dietary changes, regular exercise, sunlight exposure and stress management—can enhance serotonin production and improve cardiovascular health. The following sections will explore these points in more detail.
Assessing Serotonin Levels
It’s important to check serotonin levels, especially in people who show both heart-related symptoms and mood issues. Understanding how these factors interact is key to making a thorough assessment and creating a good treatment plan. Although direct tests for serotonin in the blood are not usually done because of its complex nature, there are other ways to gain useful information about its impact on heart health. For example, measuring the levels of a serotonin byproduct called 5-hydroxyindoleacetic acid (5-HIAA) in urine can indicate how much serotonin is being produced in the body. Additionally, checking levels of inflammatory markers and other neurotransmitters can provide a clearer view of a patient’s overall health. By understanding these connections, healthcare professionals can better customize treatments—whether through medication or lifestyle changes—to effectively address both mood and heart health for improved results.
Pharmacological Interventions
Pharmacological interventions, particularly serotonin reuptake inhibitors (SSRIs), are commonly prescribed for depression and anxiety. While these medications focus primarily on alleviating mood symptoms, they may also offer additional cardiovascular benefits. Research suggests that SSRIs can help reduce inflammatory markers, which may mitigate cardiovascular risks associated with chronic inflammation. Furthermore, by enhancing serotonin signaling, SSRIs may improve endothelial function, playing a positive role in blood pressure regulation. These potential benefits underscore the importance of considering SSRIs not only for their effects on mental health but also for their broader implications for cardiovascular well-being.
Lifestyle Modifications
Addressing serotonin deficiency must not rely solely on pharmacological interventions. Lifestyle changes can markedly improve serotonin levels and cardiovascular health:
- Diet: Foods rich in tryptophan (the precursor to serotonin), such as eggs, salmon, nuts and seeds, can help boost serotonin levels.
- Exercise: Regular physical activity is one of the most effective ways to enhance serotonin production. Exercise promotes blood flow and stimulates the release of serotonin and other mood-enhancing neurotransmitters. Engaging in activities such as aerobic exercise, yoga or even daily walking can lead to improvements in mood and overall cardiovascular health. Aim for at least 150 minutes of moderate-intensity exercise per week to reap significant benefits.
- Sunlight Exposure: Natural light helps boost serotonin levels. Spending time outdoors, especially during the morning hours, can enhance mood
 and increase the production of serotonin in the brain. Aim for 15-30 minutes of sunlight exposure daily for best results.
and increase the production of serotonin in the brain. Aim for 15-30 minutes of sunlight exposure daily for best results. - Stress Management: Techniques such as mindfulness, meditation and deep breathing exercises can help manage stress levels, thereby supporting serotonin production. Lower stress levels contribute to better overall health and can reduce the risk of stress-related cardiovascular issues.
- Sleep Hygiene: Quality sleep is essential for maintaining serotonin levels. Establish a regular sleep schedule, create a restful environment and practice good sleep hygiene to ensure adequate rest. Aim for 7-9 hours of quality sleep each night, as sleep deprivation can negatively affect serotonin production and cardiovascular health.
- Social Connections: Nurturing relationships and fostering social interactions can significantly uplift mood and promote serotonin release. Engaging in activities with family and friends, participating in community events or even volunteering can enhance feelings of belonging and reciprocal support.
Understanding the Link Between Serotonin, Mood and Cardiovascular Health
The link between low serotonin levels and heart health is becoming clearer, highlighting the importance of looking at how serotonin deficiency can negatively affect overall well-being. By understanding the various roles serotonin plays—such as its effects on blood vessels and its connection to mood disorders—we can see why it’s essential to focus on both mental and physical health together.
Combining lifestyle changes with certain medical treatments can lead to better health results for those with serotonin deficiency. As research progresses and reveals more about how serotonin affects the body, those who are affected by serotonin deficiency will be better able to take steps to improve their overall health, leading to better heart health and emotional strength.


