Depression is a complex and multifaceted mental health disorder that affects millions of people worldwide. Among the many factors contributing to depressive symptoms, serotonin—a neurotransmitter perhaps most well-known for its ability to influence mood—plays a pivotal role. Here, we will look more closely at the intricate relationship between serotonin and depression.
Serotonin: A Multifaceted Neurotransmitter
 Serotonin, chemically known as 5-hydroxytryptamine (5-HT), is a multifaceted neurotransmitter that is found primarily in the brain, intestines and blood platelets. The body synthesizes serotonin from the amino acid tryptophan, which is obtained through the diet. Often referred to as the “feel-good” neurotransmitter, serotonin influences a wide range of physiological and psychological processes, including mood regulation, sleep patterns and appetite control.
Serotonin, chemically known as 5-hydroxytryptamine (5-HT), is a multifaceted neurotransmitter that is found primarily in the brain, intestines and blood platelets. The body synthesizes serotonin from the amino acid tryptophan, which is obtained through the diet. Often referred to as the “feel-good” neurotransmitter, serotonin influences a wide range of physiological and psychological processes, including mood regulation, sleep patterns and appetite control.
Serotonin also plays a crucial role in cognition and memory, as well as in social behavior. Its significant impact on emotional well-being means that an imbalance in serotonin levels can be linked to various mental health conditions, most notably depression. Understanding the functions of serotonin and the link between serotonin and depression is essential when exploring its role in mental health and the treatment of mood disorders.
The Role of Serotonin in Mood Regulation
The role of serotonin in mood regulation is a critical area of study when seeking to understand the mechanisms that contribute to emotional well-being. As a key neurotransmitter, serotonin influences various aspects of our mental state and overall mood. Research has consistently shown that serotonin levels can directly impact emotional stability; high levels of this neurotransmitter are linked to feelings of happiness and contentment, while lower levels are often associated with sadness and mood disturbances. This connection is particularly evident in those who experience depression, where sufferers frequently report feelings of hopelessness and despair that may arise from a serotonin deficiency.
Within the brain, serotonin interactions occur in multiple regions, including the prefrontal cortex, amygdala and hypothalamus. These areas orchestrate emotional responses, decision-making and stress regulation. When there is an imbalance in serotonin levels, it can disrupt communication within these brain circuits, potentially leading to depressive symptoms. Understanding how serotonin functions within the brain highlights its importance in maintaining mood stability mental health.
Evidence Linking Serotonin and Depression
The evidence linking serotonin and depression is substantial and multifaceted. Numerous studies have demonstrated that fluctuations in serotonin levels can significantly influence mood and emotional well-being, particularly in those who have been diagnosed with depression. There are various forms of evidence that illustrate how disruptions in serotonin levels are associated with depressive disorders.
Clinical Observations
Numerous studies have evidenced the connection between serotonin and depression. For example, people who have been diagnosed with major depressive disorder often exhibit lower serotonin levels compared to non-depressed individuals. In these subjects, biological markers indicate that serotonin transmission may be impaired, resulting in diminished mood regulation.
Antidepressant Medications
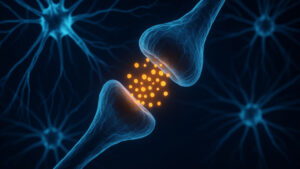
Selective serotonin reuptake inhibitors (SSRIs) represent a dominant class of antidepressant medications designed to increase serotonin levels in the brain. SSRIs, such as fluoxetine (Prozac®) and sertraline (Zoloft®), work by inhibiting the reuptake of serotonin in the synaptic cleft, thus allowing more serotonin to be available to bind to receptors. This mechanism alleviates depressive symptoms for many individuals, highlighting the neurotransmitter’s role in emotional well-being.
Neuroimaging Studies
Advanced neuroimaging techniques provide further evidence of serotonin’s involvement in depression. Functional MRI studies demonstrate altered brain activity patterns in those with depression, particularly in areas densely populated with serotonin receptors. These studies also show how SSRIs can restore normal brain function over time, further underlining the neurotransmitter’s significance in maintaining healthy mood.
The Complexity of Depression
While serotonin plays a crucial role in depression, it is essential to understand that depression is a multifaceted condition influenced by various factors.
Genetic Factors
Genetics contribute significantly to one’s susceptibility to depression. Numerous studies have shown that those with a family history of depression are at greater risk of experiencing similar issues, indicating a strong genetic link. Research has also found that specific genetic mutations can influence serotonin production and receptor sensitivity. Variations in genes related to serotonin transport and receptor functioning can lead to altered serotonin levels in the brain, increasing the likelihood of developing depression.
 Environmental Triggers
Environmental Triggers
Environmental stressors, such as trauma, significant life changes or chronic stress, can also precipitate depression. Events like the loss of a loved one, divorce, job loss or relocation can trigger profound emotional responses, sometimes leading to depressive episodes. Traumatic experiences, in particular, can leave lasting psychological effects that disrupt emotional stability. Studies indicate that trauma can enhance sensitivity to stress and alter brain chemistry, affecting serotonin levels. Chronic stress, whether from work, relationships or financial pressures, can also create ongoing emotional strain. Over time, this cumulative stress can deplete neurotransmitter reserves, further destabilizing emotional well-being. Recognizing these environmental triggers is essential for developing effective interventions and support for individuals at risk of depression.
Psychological Factors
Cognitive styles and personality traits significantly influence the development of depression. People with negative thought patterns such as pessimism, self-criticism or catastrophizing are more vulnerable to depressive symptoms. These cognitive styles can distort reality, causing a focus on failures rather than successes. Additionally, low resilience can exacerbate this vulnerability. Resilience is the ability to recover from challenges, and those with low resilience may struggle more with emotional upheaval, leading to longer periods of depression. This lack of adaptive capacity can increase sensitivity to changes in neurotransmitters like serotonin, which are crucial for mood regulation. Certain personality traits, particularly high neuroticism, can also compound the risk for depression. Recognizing these psychological factors is essential for developing effective therapeutic approaches that address both cognitive patterns and resilience, ultimately improving mental health outcomes.
Other Neurotransmitters
While serotonin is crucial, other neurotransmitters — such as dopamine, norepinephrine and gamma-aminobutyric acid (GABA) — also contribute to mood regulation. The interplay between these neurotransmitters and serotonin complicates the understanding of depression, as imbalances in multiple systems can influence one’s emotional state.
Current Treatment Approaches
Given the complexity of depression and its association with serotonin, treatment strategies can be varied and multidimensional. Pharmacotherapy remains a cornerstone of treatment, with selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) frequently prescribed to address serotonin imbalances. In addition, researchers are exploring novel antidepressants that target different aspects of serotonin function or act on alternative pathways — such as ketamine and psychedelics — which show promise in addressing treatment-resistant depression.
Another critical approach involves psychotherapy. Cognitive Behavioral Therapy (CBT) is effective in addressing the cognitive distortions often associated with depression, helping individuals to understand and alter negative thought patterns that can influence the regulation of neurotransmitters, including serotonin. Dialectical Behavior Therapy (DBT) can also play a vital role, particularly for those with emotional regulation issues, as it offers skills for managing emotions and improving interpersonal relationships.
Lifestyle modifications are equally important in the treatment of depression. Diet and nutrition can significantly impact serotonin levels; consuming foods rich in tryptophan, such as turkey, bananas and nuts, may enhance serotonin production. Additionally, omega-3 fatty acids found in fish are noted for their  mood-boosting properties. Regular exercise is also beneficial, as it increases the availability of serotonin and other endorphins, which contributes positively to mental health. Good sleep hygiene is crucial as well. Establishing a regular sleep schedule supports serotonin regulation and helps keep depression at bay.
mood-boosting properties. Regular exercise is also beneficial, as it increases the availability of serotonin and other endorphins, which contributes positively to mental health. Good sleep hygiene is crucial as well. Establishing a regular sleep schedule supports serotonin regulation and helps keep depression at bay.
There are also alternative therapies that can complement these main treatment approaches. Practices like mindfulness meditation, yoga and acupuncture can promote relaxation and reduce stress, potentially stabilizing serotonin levels. Supplementation with tryptophan or 5-HTP (5-hydroxytryptophan) is also gaining attention: Both are precursors to serotonin and may provide additional support in managing mood and emotional resilience. Together, these diverse strategies form a comprehensive framework for addressing the multifaceted nature of depression.
Serotonin and Depression: A Multidimensional Approach to Recovery
The connection between serotonin and depression is significant, yet it is only one piece of a larger puzzle. While low serotonin levels are associated with depressive symptoms, various factors — ranging from genetics to environment — can contribute to the development of this complex condition. A multimodal approach to treatment that includes medication, psychotherapy and lifestyle changes can provide sufferers with the best chance for recovery. Understanding the nuanced connection between serotonin and depression can lead to more personalized and effective treatment strategies, ultimately enhancing overall quality of life.